R evenue Cycle Management (RCM) is the lifeblood of financial health for every healthcare practice. In 2025, with tighter regulations, increased patient responsibility, and evolving payer rules, mastering the RCM process is no longer optional—it’s essential.
This guide breaks down the entire revenue cycle management process from patient registration to final payment. Whether you’re a clinic administrator, physician, or billing manager, you’ll learn how to streamline your RCM workflow and maximize revenue in today’s complex landscape.
What is Revenue Cycle Management?
Revenue Cycle Management (RCM) refers to the process of tracking and managing patient revenue from the initial appointment to the final payment. It includes everything from scheduling and eligibility verification to coding, billing, collections, and denial management.
When done right, RCM ensures:
Faster payments
Fewer claim denials
Better cash flow
Improved compliance
At MTBSRCM, we help practices turn RCM into a strategic advantage—not just a backend task.
The 9 Key Steps of the Revenue Cycle Management Process in 2025
1. Pre-Authorization and Eligibility Verification
Before care begins, verify:
Insurance coverage
Copays and deductibles
Pre-authorization requirements
Modern tools now offer real-time eligibility checks to avoid costly rejections later

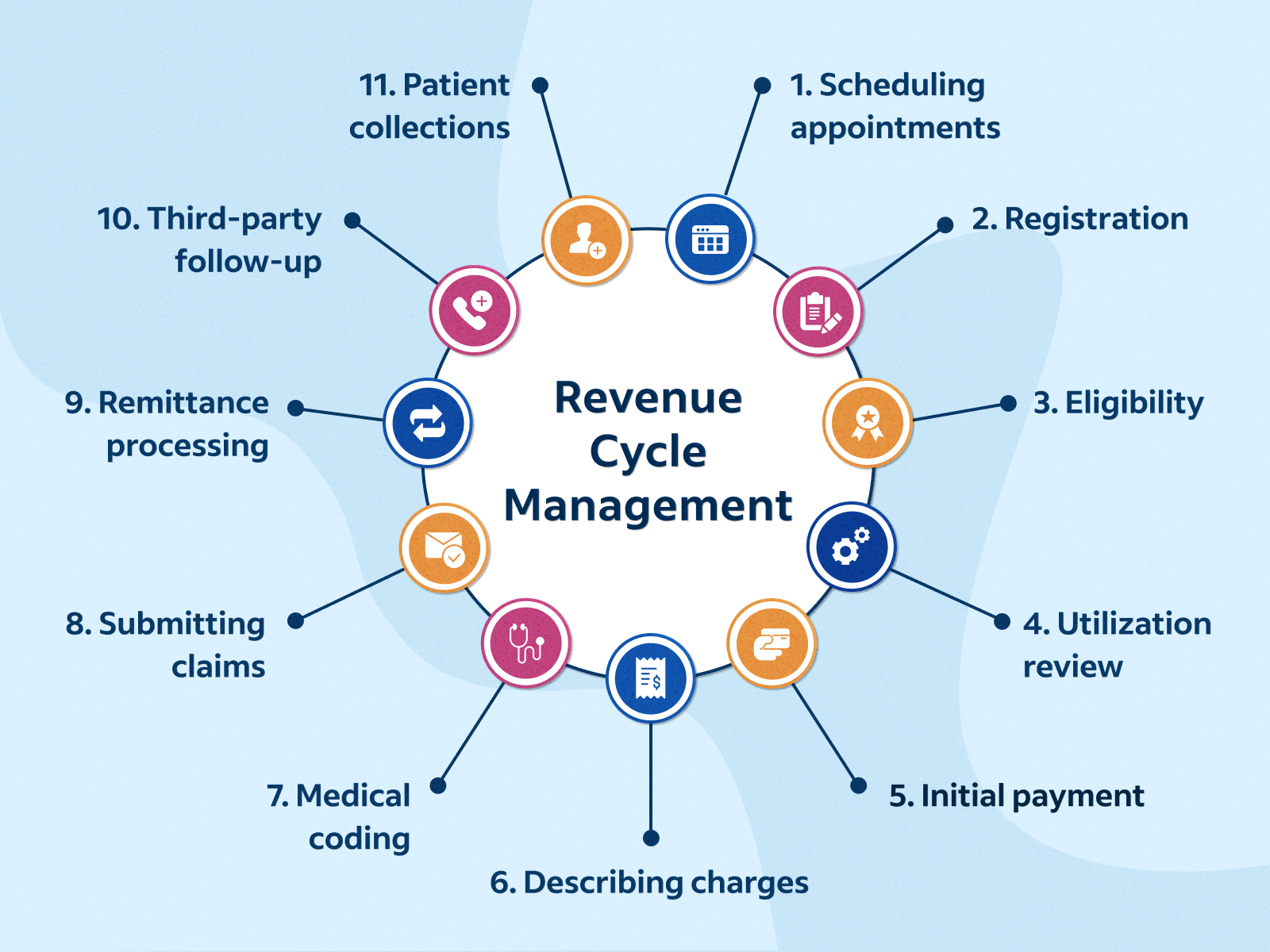
2. Patient Registration and Demographics
Accurate intake is critical. Capture:
Name, DOB, insurance ID
Contact and billing info
Referrals, if applicable
Even minor errors in this step can delay claims or lead to denials.
3. Medical Coding and Charge Entry
Coding teams assign ICD-10, CPT, and HCPCS codes based on the services provided. These codes form the foundation of your claims.
In 2025, AI-assisted coding is streamlining accuracy and compliance.
4. Claim Submission
Claims are submitted electronically to insurance payers. Clean claims = faster payouts. Outsourced billing companies ensure:
Clean format
Payer-specific requirements met
Proper modifiers used
5. Payment Posting
Once payers respond, payments and EOBs (Explanation of Benefits) are posted in the system. This helps track:
Paid amounts
Denials
Outstanding balances
This step is also crucial for reconciling with expected reimbursements.
6. Denial Management
If claims are denied, prompt action is key. Common denial causes in 2025 include:
Prior authorization missing
Eligibility issues
Coding errors
Advanced RCM systems now flag denials in real time and track trends for prevention.
7. Patient Billing and Follow-Up
With patient responsibility increasing, clear and timely billing is essential. Best practices include:
Easy-to-read statements
Multiple payment options
SMS/email reminders
Patients expect transparency and convenience in 2025.
8. Collections and Accounts Receivable Management
AR teams follow up on:
Unpaid balances
Rejected claims
Aged receivables
Partnering with a trusted RCM provider improves collection rates without harming patient satisfaction.
Ready to improve your collections? Request a free consultation
9. Compliance and Reporting
Compliance with HIPAA, CMS, and payer regulations is non-negotiable. RCM providers also generate real-time reports and KPIs to help practices make informed financial decisions.
The Role of Technology in RCM (2025 Trends)
RCM is evolving, thanks to:
AI-powered coding tools
Integrated EHR and billing systems
Predictive analytics for denial trends
Patient portals for billing transparency
Practices that embrace tech-enabled RCM are outperforming others in efficiency and reimbursement.
Expert Insight from MTBSRCM
“RCM isn’t just about collecting payments—it’s about running a smarter, more efficient practice. At MTBSRCM, we align our services with your goals, so you can stay financially healthy while focusing on quality care.”
— MTBSRCM Team
Final Thoughts
Understanding the revenue cycle management process in 2025 is crucial for every healthcare provider. Each step—from verification to collections—impacts your practice’s financial health.
If managing all of this in-house is too overwhelming or costly, outsourcing your RCM can bring faster reimbursements, lower overhead, and greater peace of mind.
🎯 Partner with MTBSRCM and let us handle your RCM, so you can focus on what matters—your patients.
Useful Links
FAQ: Revenue Cycle Management (RCM)
Q1. What is the biggest challenge in RCM today?
A: Denials and delayed reimbursements are top challenges. Accurate coding and real-time eligibility checks are key to solving this.
Q2. How does outsourcing RCM help small practices?
A: It reduces administrative workload, cuts costs, and speeds up collections. You gain access to skilled teams and advanced tools without heavy investment.
Q3. Is RCM just about billing?
A: No. RCM covers the entire journey from patient scheduling to final payment. Billing is only one component.
Q4. How secure is outsourced RCM?
A: Providers like MTBSRCM follow strict HIPAA compliance, encrypted systems, and regular audits to ensure data security.
"In addition to prescription medications, pharmacies also offer a wide range of over-the-counter remedies to treat common health issues such as coughs, colds, allergies, and pain. These products can be a convenient and affordable alternative to prescription medications for many people."
Alisa Stanton